Tondapu Sreelekha, 8th semester
Roll no. – 135
This is online E log book to discuss our patient’s de-identified
health data shared after taking his/her/guardian’s signed informed consent.
Here we discuss our individual patient’s problems through series of inputs
from available global online community of experts with an aim to solve those
patients’ clinical problems with collective current best
evidence-based inputs. This e-log book also reflects my patient centred
online learning portfolio and your valuable inputs on comment box is welcome
I’ve been given this
case to solve in an attempt to understand the topic of “patient clinical data
analysis" to develop my competency in reading and comprehending clinical
data including history, clinical findings, investigations, and come up with
diagnosis and treatment plan.
Following is the view of my case: (history as per date of admission)
CASE
A 38-year-old female came to the OPD with
chief complaints of fever since 10 days and cough since 10
days
HISTORY OF PRESENTING ILLNESS
·
Patient was apparently asymptomatic 10 days back
when she had fever. It was of high grade,
intermittent and not associated with chills and rigor.
· She also had cough since 10 days. It was
productive and the sputum was of scanty aamount.
PAST HISTORY
·
No similar complaints
in the past.
· She got a RAT done 5 days back which was negative.
· She is a known case of hypertension since 7years for which he is taking medication.
· She is not a known case
of diabetes mellitus, TB, Asthma and epilepsy
DRUG HISTROY
·
Tab. NEBIVOLOL 2.5mg/PO/OD
·
Tab. ECOSPRIN AV (75/10)mg
PERSONAL HISTORY
· DIET- vegetarian
· APPETITE- normal
· SLEEP- Adequate
· BOWELS- Regular
· MICTURATION- Normal
· ADDICTIONS- None
· ALLERGIES- None
FAMILY HISTORY
· There is no
significant family history.
GENERAL EXAMINATION
The patient was conscious, coherent and cooperative and well oriented to
time, place and person.
She was moderately built and moderately nourished.
· No pallor
· No icterus
· No cyanosis
· No clubbing
· No generalized
lymphadenopathy
· No pedal oedema
VITALS at the time of admission
·
Temperature:
febrile
·
Pulse:
82 beats/mins
·
Blood
pressure: 110/70 mmHg
·
Respiratory
rate: 16 cycles/min
·
SpO2:
93% on room air
SYSEMIC EXAMINATION
CVS
· S1 and S2 heart
sounds heard.
· No murmurs heard.
Respiratory system
· She patient was dyspnoeic
·
Bilateral
air entry +
·
Ronchi
were heard.
CNS- Intact
Abdomen
· Soft and non-tender.
· Bowel sounds were
heard.
· No organomegaly.
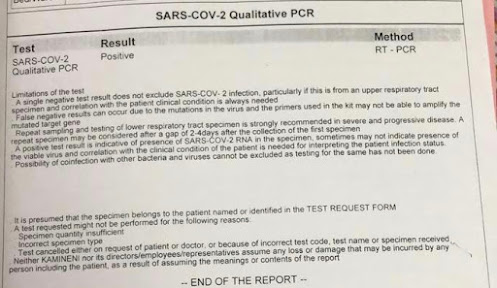
INVESTIGATIONS (day 1 of
hospitalization)
INVESTIGATIONS (day 2 of
hospitalization)
Provisional diagnosis: Viral pneumonia secondary to moderate COVID-19
infection.
Treatment given (day1)
1. Tab.
PCM 650mg/PO/TID
2. Syp.
ASCORIL 10ml/PO/BD
3. Neb
with BUDECORT – 12th hourly
4. O2
inhalation @ 4lit/hr
5. Plenty
of fluids and soft diet.
6. Tab.
NEBIVOLOL 2.5mg/PO/OD
7. Tab.
ECOSPRIN AV(75/10)mg PO/HS
8. Monitor
BP, PR, SpO2 4th hourly
Vitals (day2)
·
Temperature:
afebrile
·
Pulse:
84 beats/mins
·
Blood
pressure: 110/70 mmHg
·
SpO2:
96% on room air
Treatment given (day2)
1. Tab.
PCM 650mg/PO/TID
2. Syp.
ASCORIL 10ml/PO/BD
3. Neb
with BUDECORT – 12th hourly
4. O2
inhalation @ 4lit/hr
5. Plenty
of fluids and soft diet.
6. Tab.
NEBIVOLOL 2.5mg/PO/OD
7. Tab.
ECOSPRIN AV(75/10)mg PO
8. Monitor
BP, PR, SpO2 4th hourly
9. Inj.
CLEXANE 40mg/s.c./BD
Vitals (day3)
·
Temperature:
afebrile
·
Pulse:
94 beats/mins
·
Blood
pressure: 120/70 mmHg
·
GRBS:
8am: 171mg/dL; 4am: 154mg/dL
·
SpO2:
98% on FiO2 40%
Treatment given (day3)
1. IVF
1 NS and 2 RL @ 150ml/hr with THIAMINE and OPTINEURON
2. Inj.
PAN 40MG/IV/OD
3. Inj.
DEXAMETHASONE 8mg/IV/OD
4. GRBS
charting 4th hourly
5. Inj.
HAI s.c. according to the sliding scale
6. Vitals
charting 4th hourly
7. Tab.
NEBIVOLOL 2.5mg/PO/OD
8. Inj.
CLEXANE 40mg/s.c./BD
Vitals (day4)
·
Temperature:
afebrile
·
Pulse:
80 beats/mins
·
Blood
pressure: 120/70 mmHg
·
GRBS:
171mg/dL
·
SpO2:
96% on room air
Treatment given (day4)
1. IVF
1 NS with OPTINEURON @ 75ml/hr
2. Inj.
PAN 40MG/IV/OD
3. Inj.
DEXAMETHASONE 8mg/IV/OD
4. GRBS
charting 4th hourly
5. Inj.
HAI s.c. according to the sliding scale
6. Tab.
NEBIVOLOL 2.5mg/PO/OD
7. Inj.
CLEXANE 40mg/s.c./BD
Vitals (day5)
·
Temperature:
afebrile
·
Pulse:
74 beats/mins
·
Blood
pressure: 110/80 mmHg
·
GRBS:
134mg/dL
·
SpO2:
96% on room air
Treatment given (day5)
1. O2
inhalation to maintiain SpO2 greater than 90%
2. IVF
1 NS with OPTINEURON @ 75ml/hr
3. Inj.
PAN 40MG/IV/OD
4. Inj.
DEXAMETHASONE 8mg/IV/OD
5. GRBS
charting 4th hourly
6. Inj.
HAI s.c. according to the sliding scale
7. Tab.
NEBIVOLOL 2.5mg/PO/OD
On day 6 0f hospitalization, the patient was found to be stable and fit for
discharge.
Treatment advice given at the time of discharge
1. Tab.
NEBIVOLOL 2.5mg/PO/OD
2. Tab.
PANTOP 40mg/PO/BD for 1 week
3. Tab.
ECOSPRIN AV(75/10)mg PO/HS
4. Tab.
LIMCEE PO/OD for 2 weeks
5. Tab
MVT PO/OD for 2 weeks
6. Tab.
APIXABAN 5mg/OD for 1 week
7. Syp.
ASCORIL 10ml/PO/BD for 4 weeks