General Medicine E-log
Thursday, August 10, 2023
General medicine Internship Real patient OSCE towards optimising clinical complexity
Saturday, July 8, 2023
43 YEAR OLD MALE WITH SEIZURES
This is an online E log book to discuss our patient's de-identified health data shared after taking her guardian's signed informed consent.
Name: Sreelekha tondapu
Roll no. - 156
Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs.This E-log also reflects my patient-centered online learning portfolio and your valuable inputs in the comment box are welcome.
I've been given this case to solve in an attempt to understand the topic of "Patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, Clinical findings, investigations and come up with a diagnosis and treatment plan
Sunday, June 25, 2023
41 YEAR OLD FEMALE WITH PAIN ABDOMEN AND FEVER
This is an online E log book to discuss our patient's de-identified health data shared after taking her guardian's signed informed consent.
Name: Sreelekha tondapu
Roll no. - 156
Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs.This E-log also reflects my patient-centered online learning portfolio and your valuable inputs in the comment box are welcome.
I've been given this case to solve in an attempt to understand the topic of "Patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, Clinical findings, investigations and come up with a diagnosis and treatment plan.
GENERAL EXAMINATION
Patient is examined in a well lit room after taking an informed consent.
She is conscious, coherent and cooperative;
Pallor present.
Bilateral pitting type of pedal edema present
No signs of icterus, clubbing, cyanosis, generalized lymphadenopathy.
Monday, June 13, 2022
SHORT CASE - A 25 year old with abdominal pain
Hall ticket no. 1701006183
This is online E log book to discuss our patient’s de-identified health data shared after taking his/her/guardian’s signed informed consent. Here we discuss our individual patient’s problems through series of inputs from available global online community of experts with an aim to solve those patients’ clinical problems with collective current best evidence-based inputs.
This e-log book also reflects my patient centred online learning portfolio and your valuable inputs on comment box is welcome
I’ve been given this case to solve in an attempt to understand the topic of “patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations, and come up with diagnosis and treatment plan.
A 25 year old male patient, a painter by occupation and a resident of nalagonda came with the chief complains of
Pain abdomen since 5 days.
HISTORY OF PRESENTING ILLNESS
The patient started consuming alcohol 5 year back due to peer pressure. Initially he used to consume 90ml of brandy every day which has now increased to 180ml everyday. Which he consumes half in the morning and half in the evening before going to sleep.
The patient started smoking 2 years back. He smokes 5 beedis per day.
The patient was apparently asymptotic 3 months back when he had abdominal pain which was towards the left upper side of the abdomen. It was insidious in onset and was of dragging type. He was admitted in a hospital was a diagnosed with acute pancreatitis and was treated for the same but was inadequate.
During this visit to the hospital he was advised to stop alcohol consumption.
As suggested by the doctor the patient stopped consuming alcohol and experienced withdrawal symptoms like tremors, irritability, aggressive behaviour. He had cravings to consume alcohol.
6 days ago there was a fight between his wife and his mother due to which he consumed alcohol (180ml brandy)
He was then brought to the hospital with the symptoms of pain in the upper left abdominal region. The pain was of squeezing type and we relieved on bending forward and aggravated on eating food. He also has 3 episodes of vomiting. The vomitus was small in quantity watery in consistency and green in colour and did not have any food particles.
He did not complain of fever, chest pain, shortness of breath or constipation
PAST HISTORY
He had a similar episode 3 months back
He is not a known case of diabetes mellitus, hypertension, epilepsy, bronchial Asthma.
PERSONAL HISTORY
Diet - Mixed
Appetite - Decreased (he has been eating only curd rice and drinking fruit juices since 3 months)
Bowel and Bladder- Regular.
Sleep - Disturbed and inadequate
No known drug/food allergies
FAMILY HISTORY
Insignificant
GENERAL EXAMINATION
Patient was examined after a well informed consent in a well lit room
The patient is conscious, coherent and cooperative and well oriented to time place and person.
He is Poorly built and nourished.
He has pallor
There are no signs of icterus, cyanosis, clubbing, generalised lymphadenopathy and edema
VITALS
Temperature- 98.7°F
Pulse rate- 90bpm
Blood pressure-120/80mmHg
Respiratory rate- 16cpm
SYSTEMIC EXAMINATION :
ABDOMINAL EXAMINATION:
INSPECTION:
Shape of the abdomen- scaphoid
Umbilicus is central and inverted.
There are no visible pulsations, peristalsis, scars, sinuses or engorged veins.
PALPATION:
There is no local raise of temperature
Tenderness is present over the epigastrium and the left hypochondriac region.
No organomegaly.
PERCUSSION:
Resonant - no free fluid present
AUSCULTATION:
Bowel sounds are heard.
RESPIRATORY SYSTEM EXAMINATION
Bilateral air entry is present
Normal vesicular breath sounds are heard.
CNS EXAMINATION:
No functional deficits
CARDIO VASCULAR SYSTEM EXAMINATION
S1 and S2 are heard. No murmurs are heard.
INVESTIGATIONS:
Serum lipase - 112 IU/L
Serum amylase - 225 IU/L
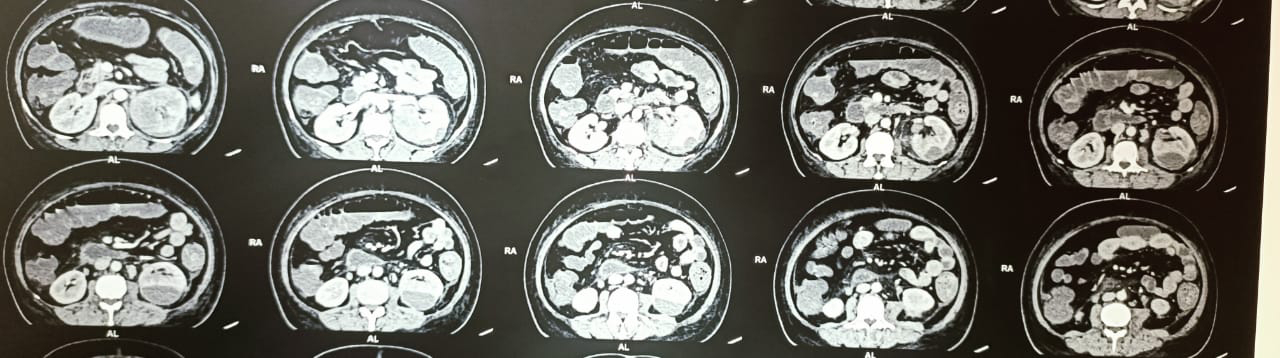
USG ABDOMEN :
findings- 5.1*2.8cms well defined anechoic cystic lesion is noted involving the body of the pancreas without internal vascularity (mostly pseudocyst)
Impression- collection noted involving body of pancreas. Likely pseudocyst.
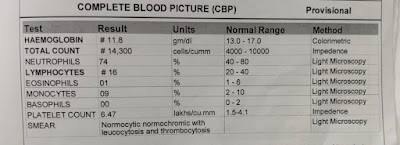
COMPLETE BLOOD PICTURE:
RENAL FUNCTION TESTS:
LIVER FUNCTION TESTS
PROVISIONAL DIAGNOSIS:
Pseudocyst of pancreas secondary to unresolved secondary acute pancreatitis with alcohol withdrawal symptoms.
Treatment
- Nil per oral (NPO)
- IV fluids RINGER LACTATE ,Normal saline 100 ml per hour
- Inj. TRAMADOL 100mg in 100ml NS IV BD
- Inj. PANTOP 40 mg IV OD
- Inj. OPTINEURIN 1 ampoule in 100ml NS IV OD
- Tab. Lorazepam 2mg BD
- Tab. Benzothiamine 100mg OD
LONG CASE- A 35 year old with shortness of breath and palpitations
This is online E log book to discuss our patient’s de-identified health data shared after taking his/her/guardian’s signed informed consent. Here we discuss our individual patient’s problems through series of inputs from available global online community of experts with an aim to solve those patients’ clinical problems with collective current best evidence-based inputs.
This e-log book also reflects my patient centred online learning portfolio and your valuable inputs on comment box is welcome
I’ve been given this case to solve in an attempt to understand the topic of “patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations, and come up with diagnosis and treatment plan.
A 35 year old male patient, bartender by occupation and a resident of sathepally presented to the OPD with the chief complaints of
- Shortness of breath since 1 month
- Palpitations since 7 days
- Pedal oedema since 2 days
- Cough since 2 days.
HISTORY OF PRESENTING ILLNESS :
The patient was apparently asymptomatic 1 month back when he started having shortness of breath which was initially of grade 2 (NYHA classification) - slight limitation of activity -ordinary activity results in fatigue. Which aggravated to grade 3 (marked limitation of physical activity- less than ordinary activity causes dyspnea) 10 days ago.
It later progressed to grade 4 (dyspnea at rest)
7 days ago.
The shortness of breath was aggravated on lying down and was relieved on sitting upright
The shortness of breath was associated with palpitations since 7 days.
He gives history of paroxysmal nocturnal dyspnea. During these episodes, once he wakes up he voluntarily stops himself from going back to sleep.
He also complains of pedal edema since 2 days. It was of pitting type and it was up to the level of his ankle joint.
There were no aggravating or relieving factors as such.
The patient developed cough 2 days back. It is not associated with sputum.
He doesn’t have any complains of excessive sweating, chest pain, chest tightness, fever, decreased urinary output.
He gives a history of alcohol binge 8 days ago.
PAST HISTORY:
There are no similar complaints in the past.
He is not a known case of diabetes mellitus, hypertension, epilepsy, bronchial Asthma.
PERSONAL HISTORY
Diet - Mixed
Appetite - Normal
Bowel and Bladder- Regular.
Sleep - Disturbed
No known drug/food allergies
Addictions: he has consumed alcohol everyday since the age of 20 (15years). He drinks 90-180ml of brandy everyday.
He is exposed to smoke as he works in a bar
FAMILY HISTORY
Insignificant
GENERAL EXAMINATION
Patient was examined after a well informed consent in a well lit room
The patient is conscious, coherent and cooperative and well oriented to time place and person.
He is Moderately built and nourished.
There are no signs of pallor, icterus, cyanosis, clubbing, generalised lymphadenopathy
He had pedal Edema upto his ankle joint. It was of pitting type.
Truncal obesity is seen.
VITALS:
Temperature: 98.6°F
Respiratory rate: 18 cycles per minute
Pulse rate : 160 beats per minute
Blood pressure : 110/80 mm of Hg
SYSTEMIC EXAMINATION:
CARDIO VASCULAR SYSTEM:
Inspection:
There are no chest wall abnormalities
The position of the trachea is central.
Apical impulse is not observed.
There are no other visible pulsations, dilated and engorged veins, surgical scars or sinuses.
Palpation:
Apex beat was localised in the 5th intercostal space 2cm lateral to the mid clavicular line
Position of trachea was central
There we no parasternal heave , thrills, tender points.
Auscultation:
S1 and S2 were heard
There were no added sounds / murmurs.
RESPIRATORY SYSTEM EXAMINATION :
Bilateral air entry is present
Normal vesicular breath sounds are heard.
CNS EXAMINATION:
HIGHER MENTAL FUNCTIONS-
Normal
Memory intact
CRANIAL NERVES :Normal
SENSORY EXAMINATION
Normal sensations felt in all dermatomes
MOTOR EXAMINATION
Normal tone in upper and lower limb
Normal power in upper and lower limb
Normal gait
REFLEXES
Normal, brisk reflexes elicited- biceps, triceps, knee and ankle reflexes elicited
CEREBELLAR FUNCTION
Normal function
No meningeal signs were elicited
ABDOMINAL EXAMINATION:
There is no local raise of temperature.
No tenderness
The abdomen is soft
No organomegaly.
No scars, sinuses, fistulas and engorged veins
INVESTIGATIONS:
Complete blood picture :
Hemoglobin - 12 gm%
TLC - 14,900 cells/cu.mm
(Neutrophils- 89%)
PCV - 37.9%
RDW - 16.9%
MCV -70.9fl
MCH - 22.4pg
Platelet count - 2.84 lakhs/cu.mm
RBC - 5.36 million/cu.mm
Liver function tests :
Total bilirubin - 2.32 mg/dl
Direct bilirubin - 0.02 mg/dl
SGPT - 58 IU/L
SGOT - 34 IU/L
ALP - 93 IU/L
Total protein- 6.9 g/dl
Albumin - 4.2 g/dl
Albumin / Globulin ratio - 1.5
Complete Urine Examination: Normal
Serum creatinine: 1mg/dL
Blood urea: 22mg/dL
Troponin I - 22.5ng/dL
ECG:
2D ECHO:
Report: moderate LV dysfunction (EF- 38%)
X-ray
PROVISIONAL DIAGNOSIS:
Heart failure with dilated cardiomyopathy and atrial fibrillation
Treatment:
Tab. DILTIAZAM - 30mg PO BD
Tab. CORDARONE - PO BD
Inj. LASIX - 40mg IV TID
Tab. ECOSPRIN - 150mg PO OD
Inj. CLEXANE - 60mg SC OD
Tab. CLOPITAB - 75mg PO OD.
Tab ATORVA - 50mg PO OD
Tab. AUGMENTIN - 65mg PO BD
Tab. AZITHROMYCIN - 500mg PO BD
Inj. THIAMINE - 20mg IV TID
General medicine Internship Real patient OSCE towards optimising clinical complexity
This online E-log Entry Blog is an objectively structured clinical examination method to assess the clinical competence during the course of...

-
This is online E log book to discuss our patient’s de-identified health data shared after taking his/her/guardian’s signed informed consent....
-
1) Pulmonology (10 Marks) A) Link to patient details: https://soumyanadella128eloggm.blogspot.com/2021/05/a-55-year-old-f...
-
This is online E log book to discuss our patient’s de-identified health data shared after taking his/her/guardian’s signed informed consent....