Hall ticket no. 1701006183
This is online E log book to discuss our patient’s de-identified health data shared after taking his/her/guardian’s signed informed consent. Here we discuss our individual patient’s problems through series of inputs from available global online community of experts with an aim to solve those patients’ clinical problems with collective current best evidence-based inputs.
This e-log book also reflects my patient centred online learning portfolio and your valuable inputs on comment box is welcome
I’ve been given this case to solve in an attempt to understand the topic of “patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations, and come up with diagnosis and treatment plan.
A 25 year old male patient, a painter by occupation and a resident of nalagonda came with the chief complains of
Pain abdomen since 5 days.
HISTORY OF PRESENTING ILLNESS
The patient started consuming alcohol 5 year back due to peer pressure. Initially he used to consume 90ml of brandy every day which has now increased to 180ml everyday. Which he consumes half in the morning and half in the evening before going to sleep.
The patient started smoking 2 years back. He smokes 5 beedis per day.
The patient was apparently asymptotic 3 months back when he had abdominal pain which was towards the left upper side of the abdomen. It was insidious in onset and was of dragging type. He was admitted in a hospital was a diagnosed with acute pancreatitis and was treated for the same but was inadequate.
During this visit to the hospital he was advised to stop alcohol consumption.
As suggested by the doctor the patient stopped consuming alcohol and experienced withdrawal symptoms like tremors, irritability, aggressive behaviour. He had cravings to consume alcohol.
6 days ago there was a fight between his wife and his mother due to which he consumed alcohol (180ml brandy)
He was then brought to the hospital with the symptoms of pain in the upper left abdominal region. The pain was of squeezing type and we relieved on bending forward and aggravated on eating food. He also has 3 episodes of vomiting. The vomitus was small in quantity watery in consistency and green in colour and did not have any food particles.
He did not complain of fever, chest pain, shortness of breath or constipation
PAST HISTORY
He had a similar episode 3 months back
He is not a known case of diabetes mellitus, hypertension, epilepsy, bronchial Asthma.
PERSONAL HISTORY
Diet - Mixed
Appetite - Decreased (he has been eating only curd rice and drinking fruit juices since 3 months)
Bowel and Bladder- Regular.
Sleep - Disturbed and inadequate
No known drug/food allergies
FAMILY HISTORY
Insignificant
GENERAL EXAMINATION
Patient was examined after a well informed consent in a well lit room
The patient is conscious, coherent and cooperative and well oriented to time place and person.
He is Poorly built and nourished.
He has pallor
There are no signs of icterus, cyanosis, clubbing, generalised lymphadenopathy and edema
VITALS
Temperature- 98.7°F
Pulse rate- 90bpm
Blood pressure-120/80mmHg
Respiratory rate- 16cpm
SYSTEMIC EXAMINATION :
ABDOMINAL EXAMINATION:
INSPECTION:
Shape of the abdomen- scaphoid
Umbilicus is central and inverted.
There are no visible pulsations, peristalsis, scars, sinuses or engorged veins.
PALPATION:
There is no local raise of temperature
Tenderness is present over the epigastrium and the left hypochondriac region.
No organomegaly.
PERCUSSION:
Resonant - no free fluid present
AUSCULTATION:
Bowel sounds are heard.
RESPIRATORY SYSTEM EXAMINATION
Bilateral air entry is present
Normal vesicular breath sounds are heard.
CNS EXAMINATION:
No functional deficits
CARDIO VASCULAR SYSTEM EXAMINATION
S1 and S2 are heard. No murmurs are heard.
INVESTIGATIONS:
Serum lipase - 112 IU/L
Serum amylase - 225 IU/L
USG ABDOMEN :
findings- 5.1*2.8cms well defined anechoic cystic lesion is noted involving the body of the pancreas without internal vascularity (mostly pseudocyst)
Impression- collection noted involving body of pancreas. Likely pseudocyst.
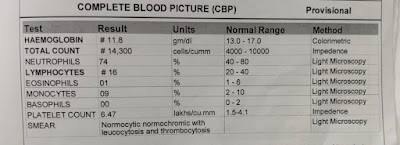
COMPLETE BLOOD PICTURE:
RENAL FUNCTION TESTS:
LIVER FUNCTION TESTS
PROVISIONAL DIAGNOSIS:
Pseudocyst of pancreas secondary to unresolved secondary acute pancreatitis with alcohol withdrawal symptoms.
Treatment
- Nil per oral (NPO)
- IV fluids RINGER LACTATE ,Normal saline 100 ml per hour
- Inj. TRAMADOL 100mg in 100ml NS IV BD
- Inj. PANTOP 40 mg IV OD
- Inj. OPTINEURIN 1 ampoule in 100ml NS IV OD
- Tab. Lorazepam 2mg BD
- Tab. Benzothiamine 100mg OD













No comments:
Post a Comment