This is online E log book to discuss our patient’s de-identified health data shared after taking his/her/guardian’s signed informed consent. Here we discuss our individual patient’s problems through series of inputs from available global online community of experts with an aim to solve those patients’ clinical problems with collective current best evidence-based inputs.
This e-log book also reflects my patient centred online learning portfolio and your valuable inputs on comment box is welcome
I’ve been given this case to solve in an attempt to understand the topic of “patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations, and come up with diagnosis and treatment plan.
A 27 year old male patient, who is a driver by occupation and a resident of Chityala came with the chief complaints of
Abdominal pain since 5 days
Nausea and committing since 5 days.
The patient was apparently asymptotic 10 years back. He started drinking at an age of 17 years. He had his first drink (toddy) in a function that he attended. At that time he consumed 2 bottles of toddy. The patient gives history that he faced similar complaints back then that is abdominal pain, nausea and vomiting. For which he was taken to the hospital and was treated.
Later the patient started drinking occasionally usually with his friends or during festivals (1 bottle)
10 days before the symptoms started the patient gives a history of drinking 1-2 bottle of toddy everyday as it was someone’s wedding/ function. The day after drinking he would wake up with a hangover and drink 1/4 bottle of toddy to get relieved from the symptoms. 5 days ago the patient gives history of going to a wedding where he ate “masala rice” and drank 2 bottles of toddy.
6 hours after this he started experiencing abdominal pain in the epigastric and the umbilical region. The pain was sudden in onset and constant throughout the time. There were no aggravating or relieving factors as such.
The patient also complains of nausea and vomiting. He has had a vomiting episode everytime he has tried to consume food.
He also had FEVER which was low-grade, intermittent , associated with burning micturition but not associated with chills& rigors cold , cough, weakness ,joint pains
As his symptoms were not subsiding he went to a hospital in nalagonda, where he was given symptomatic treatment. And was put on NBM.
He has had 2 loose stool of day 3 and day 4 of symptoms.
As the patient’s condition was not improving they shifted to our hospital.
PAST HISTORY
He is not a known case of DM, HTN coronary artery diseases, Asthma, TB, epilepsy.
PERSONAL HISTORY
Diet: mixed
Appetite: NIL
Bowel: normal
Bladder : normal
Sleep: disturbed
Addictions: consumes toddy
Allergies (food/drugs) : nil
GENERAL EXAMINATION
- The patient if conscious, coherent and cooperative
- He is Moderately built and moderately nourished
- NO signs of pallor, icterus, clubbing, cyanosis, generalised lymphadenopathy, pedal edema is seen
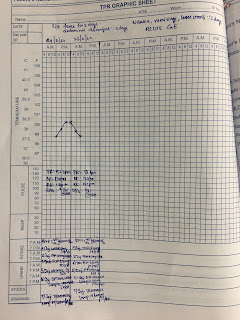
VITALS:
- PR: 90bpm
- BP: 110/70mmHg
- RR: 18 cpm
- Temperature: 99.4°F
PER ABDOMINAL EXAMINATION :
On inspection :
The abdomen is scaphoid in shape. The umbilicus was central in position and inverted.
There were no visible peristalsis, engorged veins, discoloured skin over the abdomen.
On palpation :
Tenderness is noted. Muscle guarding is present.
There is no organomegaly.
No signs of ascites.
On auscultation:
Decreased bowel sounds were heard.
Respiratory system examination
Bilateral air entry was present.
Normal vesicular breath sounds were heard.
CVS:
S1 and S2 are heard.
No abnormal heart sounds were heard.
CNS:
No fuctional deficits were noticed.
TREATMENT :
IVF : NS , RL @ 100ml/hr
INJ. ZOFER 4mg IV /BD
INJ.PANTOP 40mg IV/BD
INJ.PCM 650mg po/TID
INJ.NEOMOL 1g sos(if temp >101 f )
INJ. OPTINEURON 1amp in 100ml NS IV/BD
INJ. TRAMADOL 1amp in 100ml NS IV/BD






No comments:
Post a Comment