This is online E log book to discuss our patient’s de-identified health data shared after taking his/her/guardian’s signed informed consent. Here we discuss our individual patient’s problems through series of inputs from available global online community of experts with an aim to solve those patients’ clinical problems with collective current best evidence-based inputs.
This e-log book also reflects my patient centred online learning portfolio and your valuable inputs on comment box is welcome
I’ve been given this case to solve in an attempt to understand the topic of “patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations, and come up with diagnosis and treatment plan.
A 37 year old male, resident of yedadri district and a centring worker by occupation, came to the OPD with the chief complaints of
- Shortness of breath since 3 months
- Pedal edema since 15 days
HISTORY OF PRESENTING ILLNESS :
The patient was apparently asymptotic 3 years ago when he had fever and an episode of giddiness for which he went to the hospital and was diagnosed with hypertension.
The patient was given telmasartan and was sent home.
The patient took the medicine for few days but stopped as his relatives and friends told him not to take hypertension medication that early in life as it might lead to problems.
He used to experience neck pain during some days for which he takes the hypertensive medication apart from that he is not compliant with the medication.
Patient gives a history of shortness of breath (grade 2 MMRC) and chest pain 3 months back. The chest pain was of stabbing type and was only felt on moving from side to side or bending forward. It was also associated with a swelling over the left side of the chest (left mammary region). For this, he went to the doctor and was given medication. His complaints of pain and swelling were relieved in 3 days.
The shortness of breath was not relieved.
The patient gives history of fever 20 days back which was associated with burning micturition. The fever was of low grade and was intermittent in nature. It was associated with chills and rigor. He has had significant weight loss (the patient’s waist size decreased from 32 to 28 in the span of one month.)
He complains of pedal edema since 15 days. It initially extended till his ankle. Presently it extends up till his knee.
The shortness of breath has increased to grade 3 MMRC in the last one month due to which he stopped working. 5 days back his SOB increased to grade 4 MMRC.
PAST HISTORY
He is not a known case of DM, coronary artery diseases, Asthma, TB, epilepsy.
PERSONAL HISTORY
- Diet: mixed
- Appetite: Reduced
- Bowel: normal
- Bladder : burning micturition
- Sleep: disturbed
- Addictions: he has been consuming 90ml of whiskey everyday for the past 15 years. He has been smoking 2 cigarettes per day for the past 15 years. He also chews ghutka.
- Allergies (food/drugs) : nil
GENERAL EXAMINATION
- The patient if conscious, coherent and cooperative
- He is Moderately built and moderately nourished
- Pallor is present
- Edema upto the knee joint is seen. It is of pitting type.
- NO icterus, clubbing, cyanosis, generalised lymphadenopathy is seen
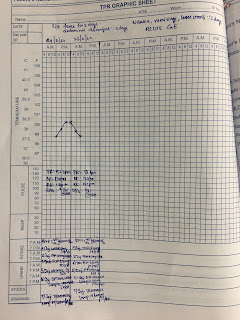
VITALS:
- PR: 90bpm
- BP: 150/100mmHg
- RR: 18 cpm
- Temperature: Afebrile
SYSTEMIC EXAMINATION
CVS:
- On palpation,
-Apex beat was diffuse and was felt at 6th intercostal space lateral as well as medial to mid-clavicular line.
-JVP was raised
-No precordial bulge
- parasternal heave was felt
- On auscultation
- S1, S2 heard; no murmurs were heard
ABDOMINAL EXAMINATION:
The abdomen is scaphoid.
Tenderness was noticed just below the sternum.
There is no local raise of temperature.
There was no organomegaly.
RESPIRATORY SYSTEM:
Bilateral air entry was present.
Vesicular breath sounds were heard.
CNS:
No functional deficits were noticed.
X-ray:
Mild pleural effusion and prominent right descending pulmonary artery
Cardiomegaly
ECG:
left ventricular hypertrophy
FUNDOSCOPY:
Right eye and left eye show grade 1 hypertensive retinopathy changes.
ULTRASOUND ABDOMEN AND PELVIS:
B/L grade 3 parenchyma disease and mild ascites was seen.
CUE
- Albuminuria present
24 hr UPCR sent
24 hr urinary protein - 1,190 mg/day
24 hr urinary sodium- 227 mmol/day
24 hr urine volume 1300ml
Serum Uric acid- 7.5 mg%
Serum electrolytes Na - 140, Cl 106, K+ 5
Serum creatinine- 5.6 mg/dl
Serum calcium- 9mg/dl
Blood urea - 119 mg/dl
2D echo
All chambers are dilated.