This is an online E log book to discuss our patient's de-identified health data shared after taking her guardian's signed informed consent.
Name: Sreelekha tondapu
Roll no. - 156
Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs.This E-log also reflects my patient-centered online learning portfolio and your valuable inputs in the comment box are welcome.
I've been given this case to solve in an attempt to understand the topic of "Patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, Clinical findings, investigations and come up with a diagnosis and treatment plan.
A 41 year old patient came to the casualty with
CHIEF COMPLAINTS:
1. Pain abdomen since 2 months
2. Fever since 2 months
HISTORY OF PRESENTING ILLNESS:
Patient came to the casualty with complains of pain abdomen since five days
The patient was apparently asymptomatic 2 years back when she had white discharge PV for which she took medication but it did not resolve. She had a surgery (hysterectomy) for the same on April 26 2023.
Since then the patient was having on and off episodes of pain abdomen which was of squeezing type and diffuse. It was relieved on taking medication (unknown)
Since five days, the intensity of pain has increased. The pain in the hypogastric region and is of squeezing type. She also complains of pain in the left lower back region which is of squeezing type and radiates towards the groin.
It is associated with vomitings (2 to 3 episodes per day, non-projectile, non-bilious, watery with food particles as contents.)
The patient also complains of fever on and off since two months which is of low grade, intermittent and is associated with chills and rigours and reduced on taking medication (paracetamol 650mg PO/BD)
The patient complains of burning micturition since 2 months.
No Complains of decreased urine output.
PAST HISTORY :
- Patient was diagnosed with DM2 four days back and not put on any medication
- Not a known case of HYPERTENSION, TUBERCULOSIS, CVA, CAD, THYROID DISORDERS, BRONCHIAL ASTHMA.
MENSTRUAL HISTORY
Past: attained menarche at 12 years
3/30, 2-3 pads/day
Present:
Hysterectomy done on April 26/04/23
Marital history:
Age of marriage: 15 years
Non consanguineous marriage.
Obstetric history:
P2A2L1D1:
A1: Spontaneous abortion at 5 months
D1: still born
A2: elective abortion done at 4 months dur to severe IUGR
L1: 9years, Female, 3 kgs at birth, NVD, Alive and healthy
PERSONAL HISTORY
Diet: mixed
Sleep: adequate
Bowel and bladder: regular
Addictions: the patient drinks toddy during festivals
Allergies: nil
Family history: not significant
Patient is examined in a well lit room after taking an informed consent.
She is conscious, coherent and cooperative;
Pallor present.
Bilateral pitting type of pedal edema present
No signs of icterus, clubbing, cyanosis, generalized lymphadenopathy.
VITAL AT THE TIME OF ADMISSION: (24/06/23)
BP: 160/90 mm of hg
PR: 121 bpm
RR: 24cpm
Spo2: 99% at RA
Systemic examination:
ABDOMINAL EXAMINATION:
On inspection:
-Truncal obesity is seen.
-Umbilicus is central and inverted.
- well healed transverse scar is seen on the lower abdomen.
-There are no visible pulsations, peristalsis, sinuses or engorged veins.
PALPATION:
-There is no local raise of temperature
-Tenderness is present over the hypogastric region.
- left renal angle tenderness present
- Abdomen is soft
-No organomegaly.
AUSCULTATION:
Bowel sounds are heard.
RESPIRATORY SYSTEM EXAMINATION
-Bilateral air entry is present
- decreased breath sounds in ISA and IAA
CNS EXAMINATION:
No functional deficits
CARDIO VASCULAR SYSTEM
S1 and S2 are heard. No murmurs are heard
Provisional diagnosis:
Acute left pyelonephritis with lower pole abscess of left kidney with ?LRTI with normocytic normochromic anaemia with De novo DM II
INVESTIGATIONS DONE PRIOR TO ADMISSION
INVESTIGATIONS 24/06/23
RBS: 101 mg/dl
Serum urea: 15 mg/dL
Serum Creatinine: 0.8 mg/dL
Serum electrolytes
Na+: 136 mEq/L
K+: 2.9 mEq/L
Cl-: 102 mEq/L
Ca2+ (ionized) : 1.09 mmol/L
Urine electrolytes
Na+: 126 mEq/L
K+: 6.9 mEq/L
Cl-: 139 mEq/L
LFT
total billirubin : 0.58 mg/dL
Direct bilirubin: 0.15 mg/dL
AST: 29 IU/L
ALT: 16 IU/L
ALP: 297* IU/L
Total proteins: 4.6 gm/dL
Albumin: 1.7gm/dL
A/G ratio: 0.57
PT: 17
INR: 1.25
APTT: 35
Hemogram:
Hb: 7.5gm/dL*
Total count: 12,500 cell/mm3*
N/L*/E/M/B: 80/15*/3/2/0
PCV: 22.2vol%*
MCV: 71.6fl*
MCH: 24.2pg*
MCHC: 33.8%
RDW-CV:14.8 %*
RBC COUNT: 3.1 millions/mm3*
PLATELET COUNT: 2.4 lakhs/mm3
Smear
RBC: normocytic Normochromic
WBC: leukocytosis
Platelets: adequate in number and distribution
HEMOPARASITES: no hemoparasites seen
IMPRESSION: microcytic hypochromic anemia
Serology : negative
CUE:
Albumin: +
Sugars: nil
Bile salts/ bile pigments : nil
Pus cells: 2-3 cells /hpf
Epithelial cells: 2-3 cells/hpf
No crystals, casts, red blood cells.
Urine for ketone bodies: negative
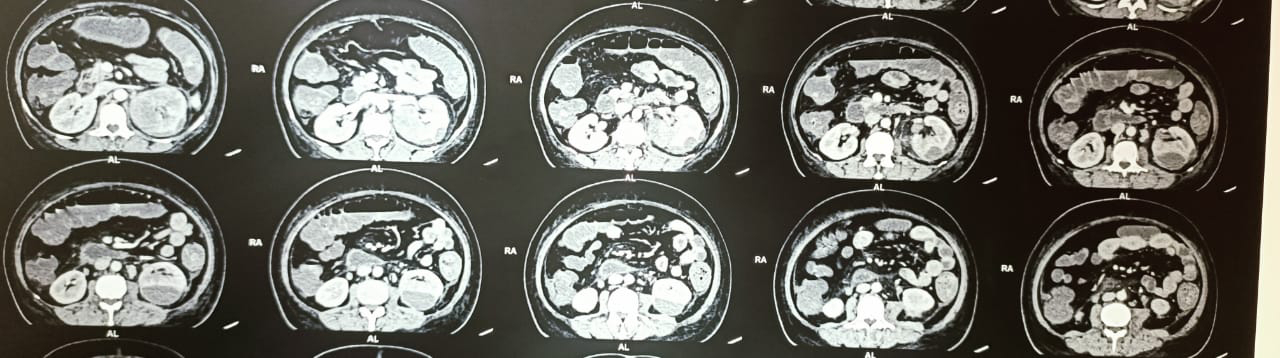
USG ABDOMEN AND PELVIS:
FINDINGS:
1. Evidence of bulky and altered echotexture of left kidney with perinephric fluid
2. Evidence of 42*35mm hypoechoic area noted in lower pole of left kidney with no internal vascularity (? Abscess)
IMPRESSION:
Left pyelonephritis with abscess in the lower pole of the kidney
ECG:
2D ECHO:
Treatment given: (24/06/23)
1. IVF NS @ 75ml/hr
2. INJ. PIPTAZ 4.5g IV/TID
3. INJ. PAN 40MG IV/OD (BBF)
4. INJ. BUSCOPAN 1AMP IM/SOS
5. INJ. TRAMADOL 1AMP IN 100ML NS IV/SOS
6. INJ. ZOFER IV/SOS
7. INJ. NEOMAL 1G IV/SOS
8. OXYGEN SUPPORT TO MAINTAIN SATURATION ABOVE 95%
25/06/23
Hemogram:
Hb: 7.9 gm/dL*
Total count: 12,000 cell/mm3*
N/L*/E/M/B: 80/16*/1/9/0
PCV: 23.3vol%*
MCV: 71.3fl*
MCH: 24.2pg*
MCHC: 33.9%
RDW-CV:15.4%*
RBC COUNT: 3.27 millions/mm3*
PLATELET COUNT: 3.15lakhs/mm3
Smear
RBC: microcytic hypochromic
WBC: leukocytosis
Platelets: adequate in number and distribution
HEMOPARASITES: no hemoparasites seen
IMPRESSION: microcytic hypochromic anemia
USG CHEST
FINDINGS:
-E/o air bronchograms seen in B/L visualized lungs feilds.
- E/o minimal free fluid Noted in left pleural space with underlying lung collapse.
- right pleural space normal
- No underlying lung collapse on the right side
IMPRESSION:
- B/L air bronchograms in B/L visualized lungs fields. - S/O consolidatory changes.
- Left minimal pleural effusion with underlying lung collapse
Reticulocyte count: 0.5%
Serum electrolytes
Na+: 133 mEq/L
K+: 2.8 mEq/L
Cl-: 98 mEq/L
Ca2+ (ionized) : 1.10mmol/L
26/06/23
Serum electrolytes
Na+: 135 mEq/L
K+: 3.2 mEq/L
Cl-: 103 mEq/L
Ca2+ (ionized) : 1.14 mmol/L
Hemogram:
Hb: 7.9 gm/dL*
Total count: 12,000 cell/mm3*
N/L*/E/M/B: 80/16*/1/9/0
PCV: 23.3vol%*
MCV: 71.3fl*
MCH: 24.2pg*
MCHC: 33.9%
RDW-CV:15.4%*
RBC COUNT: 3.27 millions/mm3*
PLATELET COUNT: 3.15lakhs/mm3
Smear
RBC: microcytic hypochromic
WBC: leukocytosis
Platelets: adequate in number and distribution
HEMOPARASITES: no hemoparasites seen
IMPRESSION: microcytic hypochromic anemia
HbA1c: 6.9%
Stool for occult blood : negative
Serum ferritin:
Review USG I/V/O liquefaction status of the abscess:
-e/o 60*36mm hypoechoic collection noted in the lower pole of the left kidney with 30-40% liquefaction status with internal echoes and septations
- e/o mild perinephric collection and peri nephric fat stranding.
Left kidney -12. 2*6.5 cms (increased size and altered echotexture)
IMPRESSION:
Left pyelonephritis with abscess in the left lower pole with 30-40% liquefaction status.
Treatment given :
1. IVF NS, RL @ 75ml/hr
2. INJ. PIPTAZ 4.5g IV/TID
3. INJ. PAN 40MG IV/OD (BBF)
4. INJ. BUSCOPAN 1AMP IM/SOS
5. INJ. TRAMADOL 1AMP IN 100ML NS IV/SOS
6. INJ. ZOFER 4MG IV/SOS
7. INJ. NEOMAL 1G IV/SOS (IF TEMP> 101F)
8. INJ. HAI S/C ACC TO GRBS
9. SYP. POTCHLOR 15ML PO/BD
27/06/23
INVESTIGATIONS
Hemogram:
Hb: 8gm/dL*
Total count: 12,700 cell/mm3*
N/L/E/M/B: 75/16*/2/7/0
PCV: 24.6vol%*
MCV: 75.5fl*
MCH: 24.6pg*
MCHC: 33.8%
RDW-CV:17.2%*
RBC COUNT: 3.25 millions/mm3*
PLATELET COUNT: 3.43 lakhs/mm3
Smear
RBC: microcytic hypochromic
WBC: leukocytosis
Platelets: adequate in number and distribution
HEMOPARASITES: no hemoparasites seen
IMPRESSION: microcytic hypochromic anemia
Serum urea: 18 mg/dL
Serum Creatinine: 0.8 mg/dL
Serum electrolytes
Na+: 134mEq/L
K+: 4.3mEq/L
Cl-: 104mEq/L
Ca2+ (ionized) : 1.03 mmol/L
URINE C/S
Treatment
1.IVF NS, RL @ 75ml/hr
2. INJ. PIPTAZ 4.5g IV/TID
3. INJ. PAN 40MG IV/OD (BBF)
4. INJ. BUSCOPAN 1AMP IM/SOS
5. INJ. TRAMADOL 1AMP IN 100ML NS IV/SOS
6. INJ. ZOFER 4MG IV/BD
7. INJ. NEOMAL 1G IV/SOS (IF TEMP> 101F)
8. INJ. HAI S/C TID BEFORE MEALS ACC TO GRBS
9. SYP. POTCHLOR 15ML PO/BD