|
Friday, January 14, 2022
Wednesday, January 12, 2022
80 year old with complaints of cough, fever, SOB and decreased urine output
This is online E log book to discuss our patient’s de-identified health data shared after taking his/her/guardian’s signed informed consent. Here we discuss our individual patient’s problems through series of inputs from available global online community of experts with an aim to solve those patients’ clinical problems with collective current best evidence-based inputs.
This e-log book also reflects my patient centred online learning portfolio and your valuable inputs on comment box is welcome
I’ve been given this case to solve in an attempt to understand the topic of “patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations, and come up with diagnosis and treatment plan.
An 80 year old patient a resident of kurumarthi presented with the chief complaints of
- cough since 15 days
- Fever since 15 days
The patient was apparently asymptomatic 10 years back when he developed throbbing pain in his right meta-tarso phalangeal joint. It was also associated with swelling of the joint and fever. 2 weeks Later he also had swelling and pain in bilateral knee joints. With these symptoms the patient went to a nearby hospital. On evaluation in the hospital he was informed to have increased Uric acid (as informed by the attender) and was diagnosed with gouty arthritis; treatment was started started for the same (drugs taken- unknown). He was diagnosed with CKD during this visit.
During the same visit he was diagnosed with hypertension and medication was given.(stamlo 2.5mg OD). He has been compliant with the medication till date.
After 2 weeks of using the medication for gouty arthritis the patient symptoms increased and progressed to involve his bilateral hip joints, shoulder joints, MCP, DIP and PIP. After which he stopped the medication prescribed to him and switched to homeopathic medication.
His symptoms subsided with the prescribed homeopathic medication and he was compliant with them.
He used to have exacerbation of the gout when he consumes red meat or any pulses. He used to have 2 exacerbation in an year, during these episodes he used to take a higher dose of the homeopathic medication.
The patient stopped working in the field due to his severe symptoms.
Over the course of 10 years the patient’s lifestyle was severely effected. He started using a stick to help him walk 8 years back and started using a four legged stand 6 years back.
He stopped using homeopathic medication 3 years ago as his symptoms of pain and swelling in the joints reduced. During the episodes of exacerbations, he used to take a paracetamol which relieved his symptoms.
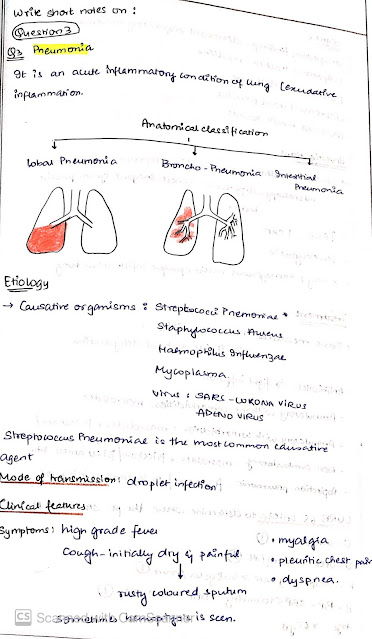
- The patient complains of cough since 15 days. It was associated with sputum which was profuse, viscous, pale-yellow coloured, non- blood tinged and non-foul smelling. There is no diurnal and positional variation.
- He has had high grade fever since 15 days which is not associated with chills or rigor.
- He also complains of shortness of breath since 15 days. Which initially started as grade 2 MMRC classification (shortness of breath after walking 100m) later progressed to grade 4 MMRC classification (shortness of breath at rest). He didn’t have orthopnea, paroxysmal nocturnal dyspnea, chest pain and palpitations.There were no aggravating or relieving factors as such.
- He has decreased urine output since 3 days.
The patient was taken to an hospital in Hyderabad 8 days back where he had one round of dialysis ( reason for dialysis: unknown. According to the attender the creatinine was high)
He later came to our hospital for further dialysis.
PERSONAL HISTORY :
He take a mixed diet, his appetite has decreased since the past 15 days.
His bowel movements are regular
He has decreased urine output.
His sleep is disturbed due to cough.
He used to smoke 20 chutas/ day. He started smoking at the age of 17. He stopped smoking after being diagnosed of gout 10 years back.
He consumes alcohol occasionally (30ml whiskey)
He doesn’t have any know food allergies or drug allergies
FAMILY HISTORY:
No history of coronary vascular diseases, cancer, epilepsy, cerebral vascular diseases.
GENERAL EXAMINATION:
Patient is drowsy and easily arousable.
Moderately built and poorly nourished
Pallor is present
Mild bilateral pitting type of pedal edema is present
No icterus, clubbing, cyanosis, generalised lymphadenopathy is seen
VITALS:
PR: 82bpm
BP: 110/80 mmHg
RR: 20cpm
Temperature: Afebrile
SYSTEMIC EXAMINATION
RESPIRATORY SYSTEM :
INSPECTION:
bilaterally symmetrical
Expansion of chest: Decreased on left side
Position of trachea: Central
Supraclavicular and infraclavicular hollowness seen
Spinoscapular distance could not be measured
Muscle wasting seen over supraclavicular area
Crowding of ribs seen
Retraction of intercostal muscles seen on respiration
No visible scars, sinuses, pulsations
PALPATION:
Inspectory findings confirmed
No tenderness, local rise of temperature
Decreased expansion of chest on left side in all areas
Chest diameter: AP- 27cm ; Transverse- 23cm
Position of trachea: Central
Vocal fremitus: resonant note felt
PERCUSSION:
Dull note heard over Left infraclavicular, mammary and inframmary areas
Posterior side not percussed
Other areas- resonant note heard
AUSCULTATION:
Bilateral crepts heard over mammary, inframmary areas
Decreased breath sounds bilaterally
Vocal resonance: resonant in all areas
CVS:
On palpation,
-Apex beat felt at 5th intercostal space along midclavicular line
-JVP not raised
-No precordial bulge
-No parasternal heave
On percussion, the heart borders were in normal limits
On auscultation, S1, S2 heard; no murmurs
P/A:
Soft, non-tender
No hepato-spleenomegaly noted
CNS:
HIGHER MENTAL FUNCTIONS-
Altered sensorium seen
Drowsy and (?)
Speech and language normal
Memory intact
CRANIAL NERVES-
1, 9,10,11, 12: Could not be elicited due to O2 mask
Other cranial nerves are normal
MOTOR EXAMINATION-
Normal bulk in upper and lower limbs
Normal tone in upper and lower limbs
Normal power in upper and lower limbs
Gait could not be examined
SENSORY EXAMINATION-
Normal sensations felt in all dermatomes
REFLEXES-
Normal, brisk reflexes elicited- biceps, triceps, knee and ankle reflexes elicited.
CEREBELLAR FUNCTION-
Normal function
No meningeal signs were elicited.
EVALUATION:
Fever chart
RENAL FUNCTION TEST:
X- ray chest
LIVER FUNCTION TEST:
Hemogram:
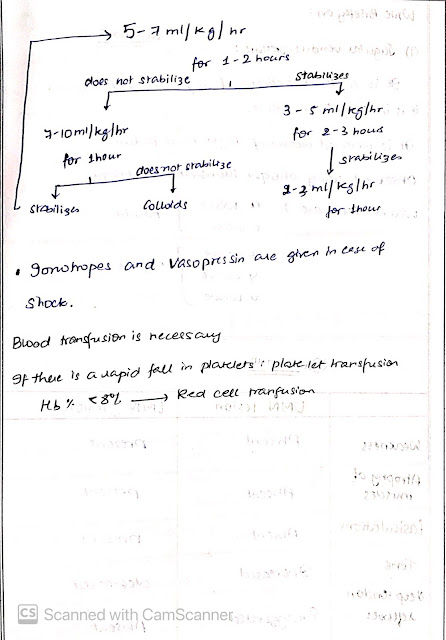
Treatment plan :
Day 1 of hospitalisation:
10/1/22
P:
TREATMENT GIVEN
INJ.PAN 40 MG /IV/OD
INJ.ZOFER 4 MG /IV/SOS
IVF - NS @ UO+50 ML/HR
INJ .LASIX 20 MG /IV/BD
TAB PCM 650 MG /RT/SOS
INJ PIPTAZ 2.25 G /IV/TID
BP/PR/TEMP MONITORING 4TH HOURLY
GRBS CHARTING 12 TH HOURLY
2nd hourly oral suctioning
General medicine Internship Real patient OSCE towards optimising clinical complexity
This online E-log Entry Blog is an objectively structured clinical examination method to assess the clinical competence during the course of...

-
This is online E log book to discuss our patient’s de-identified health data shared after taking his/her/guardian’s signed informed consent....
-
1) Pulmonology (10 Marks) A) Link to patient details: https://soumyanadella128eloggm.blogspot.com/2021/05/a-55-year-old-f...
-
This is online E log book to discuss our patient’s de-identified health data shared after taking his/her/guardian’s signed informed consent....